
Here, we delve further into the stories that bring our strategy to life and show real examples of how our clinical vision is already delivering for our patients.
You can read our clinical strategy, Bringing the best of the NHS to every patient, in full by clicking the button below.
Our group priorities
We have identified three key clinical priorities which all our hospitals and sites will focus on to deliver the best possible care for our patients: cancer, cardiovascular, and organ failure and transplantation.
The Royal Free London (RFL) plays a leading role in these areas within north central London and beyond, and they have a significant impact on the health of our local populations.
Cancer
As one of the largest cancer care providers in the UK, the RFL is already at the heart of tackling this devastating disease.
Learn more about how our nuclear medicine team is helping to diagnose cancer faster than ever before thanks to skilled staff and new technology.
The nuclear medicine team is a shining examp
The team uses radioactive material to diagnose and treat a range of diseases. Several techniques are used and the team consists of doctors, technologists, radiopharmacists, physicists, radiographers, healthcare assistants and administrative staff.
Leading the team is Danny McCool, head of nuclear medicine.
“Where the strength of the department comes from is its multidisciplinary nature,” Danny said. “Each of our skill sets are quite different and we all challenge and adapt to each others’ requirements on every day.
“The technology is really exciting in nuclear medicine, but new pharmaceutical, mathematical and physics techniques are always coming through which means we can push the boundaries even further.”
Earlier this year an £8m positron emission tomography (PET) scanner – the first of its kind in the NHS – was installed at the Royal Free Hospital (RFH) which allows the team to deliver more accurate and faster diagnoses. It is 11 times more sensitive than the latest standard machines and will help diagnose lymphoma, neuroendocrine tumours, colorectal, skin and lung cancers at a much quicker rate than ever before.
Danny describes the scanner as a ‘host of information’.
“If different parameters are derived from patient data, we can really discover information on a cellular level that was previously unavailable to us,” he said. “The physics team is very well placed to exploit this data, with their mathematical, statistical and coding skills."
“We’re also the biggest centre for radionuclide therapy in the UK, and with our own pharmacy and state-of-the-art PET centre we are positioned to be even stronger going forward.”
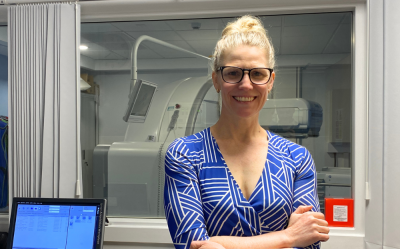
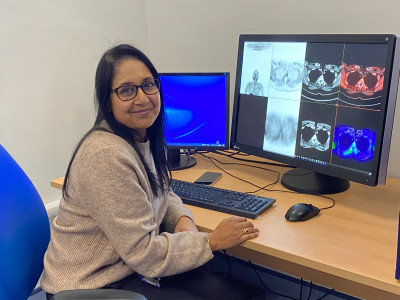
Dr Malavika Nathan, consultant nuclear medicine physician and radiologist, is the co-clinical lead for nuclear medicine.
“Nuclear medicine has expanded hugely in the past 20 years,” Malavika said. “That expansion has mainly taken place over the past 10 years, in terms of the number of cameras, staffing and the size of the department.
“We are embedded in the oncology service. So many cancer patients will at some point during their treatment come into contact with us, and we have a heavy presence within multidisciplinary team meetings for the further care of the patient.
“We also see research as a new frontier for the department, and with academic posts coming along with the scanner, we will be able to take that forward,” Malavika added.
Amy Pritchard, chief nuclear medicine technologist, says that her day-to-day role is a “little bit of everything”. She manages a large team of technologists and support staff and is heavily involved in recruitment to the department, which can be a challenge in the UK.
“In most other countries nuclear medicine is an option you can do right after university,” Amy said. “To give context – of 30 colleagues here in the department, just one has a British passport, so we are truly an international team.
“With the new scanner, I have had quite a few roles to recruit to which is really exciting but that can also bring challenges as it takes over a year to train someone new.”
The new scanner brings with it a range of benefits for staff experience.
“Up until this year we were a single-scanner department, and we were scanning more patients that any other similar department in the UK which shows how hard colleagues have been working,” Amy said.
“Technologists can see more patients in a shorter period of time, and our capacity has been futureproofed. The admin staff can now open the diary and book a slot without the need for active cancellation lists, making for a nicer environment to work in.”
Ivy Vito, deputy chief nuclear medicine technologist, is one of the team members who has expanded her skill set to create a better experience for patients. She has been involved in the area of radionuclide therapy since 2013, which was previously solely the remit of consultants and physicists.

“That would mean that patients would have to wait for blood tests before starting therapy, which could take a few hours and overall lengthen the working day for the team,” Ivy said.
“Now we can send for urgent blood tests and get quick results, and instead of waiting for the cannulation team, I can get started almost immediately which reduces the time the patient has to wait.”
Ivy also reports bone density (DEXA) scans, which were previously only carried out by consultants, and ensures that the team remain up to date with changes in nuclear medicine using a quality management system.
“There is no blaming culture in this department. If there is a mistake, we capture it, talk about it and find out how we can improve as a team, which I am really proud of.”
Cardiovascular
Cardiovascular disease remains one of the leading causes of death in the UK and within north London. North central London also has high rates of smoking, alcohol consumption and obesity, which all contribute to cardiovascular disease.
Learn about how patients at Barnet Hospital (BH) are receiving the best cardiovascular care at home thanks to virtual wards.

Patients with heart failure at Barnet Hospital (BH) are accessing consultant-led care from the comfort of their own home, thanks to a ‘virtual ward’ project aimed at helping them recover faster.
Following an assessment to check they are stable, suitable patients are discharged home with a blood pressure monitor and medical-grade scales. They are asked to enter their results into an app each day and the results, along with any symptoms, are monitored by the cardiology team.
Where needed, medication can be adjusted, with doctors available over the phone to respond to any concerns.
Nicolas Karpasitis, 42, from Barnet, says for him the experience has been nothing but positive. He came to BH’s emergency department with breathing problems related to an enlarged heart.
He said: “The cardiology team have been brilliant and I found it really interesting to monitor my own health – in fact I’ve enjoyed playing a role in my recovery. At one point I did have to come back in as an inpatient, but the majority of time was spent at home. When I was finally discharged off the virtual ward it felt a bit sad actually, it felt like losing a friend as I enjoyed chatting to the team. Now I continue to be monitored but not as intensely.”

Dr Nelson Amaral, the consultant cardiologist behind the project, said: “We recognised that a virtual ward could be a perfect fit for heart failure patients. These patients often experience lengthy hospital stays, but in many cases, close monitoring can be effectively conducted from at home where they can enjoy a better night’s sleep. As we know, familiar surroundings are a significant factor in patient wellbeing.”
The virtual ward utilises a user-friendly app to monitor weight, blood pressure, and any other relevant symptoms. This allows the team to promptly adjust medication as needed. Strict criteria are in place, patients must be medically stable and have the capacity to actively participate in their care. Access to a smartphone is also a requirement.
Jennifer Lane, a heart failure clinical nurse specialist, said:
“Previously patients were waiting up to a month for their first clinic appointment and up to nine months for a follow-up appointment. Now we’re able to review patients the day after discharge from their own home. During their two weeks on the virtual ward they come in regularly for blood tests and receive medication which is rapidly increased to the top tolerated dose. Nicolas’s case was particularly complex but being on the virtual ward highlighted the issues he was facing and prevented him returning to us via A&E.
“We currently have 10 patients on the virtual ward at any one time and that number will rise.”
Although the team is still collecting and evaluating the data, they believe the results will show better outcomes for patients.
The project has been funded by the North Central London Integrated Care System (NCL ICS).
Organ failure and transplantation
Our liver and renal services attract many patients from north central London and nationally. Liver disease is on the increase nationally and moderate to severe chronic kidney disease affects around 6% of our population.
Learn about the steps we are taking to give patients the best chances of receiving and benefitting from a kidney transplant.
Kidney patients at the RFL are benefitting from a new programme which aims to help them lose weight prior to transplant.
Known as Kidney Fitness for Transplant (K-FiT), the initiative focuses on improving the length and quality of life for patients living with obesity who have end-stage kidney disease.
Due to the increased risks of surgery when overweight, patients must have a body mass index (BMI) of below 35 and moderate abdominal obesity to be considered for the national kidney transplant waiting list. The aim is to support patients to overcome the barrier of weight loss, so they fulfil the criteria to be listed.
A team made up of dietitians, physiotherapists, psychologists, pharmacists, and a kidney transplant surgeon are working together to initially support approximately 40 patients over a year.
The team offer meal and exercise plans which are tailored to each patient’s needs, along with comprehensive support for their overall wellbeing. Some patients will also receive medication to support their fitness journey.
After six months, most patients will either be listed on the kidney transplant waiting list, offered the opportunity to continue with the K-FiT programme, or provided with a fast referral for weight loss surgery.
Jacqueline Gandy, specialist chronic kidney disease dietitian, said: “Individuals living with kidney disease often need to follow strict dietary restrictions and attempting significant weight loss can also add to the challenge of managing their lifestyle. My role involves empowering individuals to enhance their knowledge, confidence, and skills to make informed dietary choices, to help them achieve their health and weight management goals.”
Mr Ammar Al Midani, consultant transplant and access surgeon, said: “K-FiT is not only about weight loss for our renal patients, it is about promoting longevity and overall wellbeing.
“Through this innovative programme, our goal is to help patients with end-stage kidney disease, either approaching dialysis or currently undergoing it, to get listed on the national kidney transplant waiting list. Having a kidney transplant will significantly improve a patient’s quality of life and enable them to get back to their daily activities.”
Over 800 patients visit our hospitals three times every week to receive dialysis – this is the process of removing excess water and toxins from the body to simulate the work of the kidney.
Our local clinical priorities
Our hospitals have different opportunities and challenges based on the patients they care for.
We have developed local clinical priorities that reflect the needs and expectations of those different communities. Below are examples of the steps we are taking to improve the health of populations across north central London and beyond.
Barnet Hospital (BH)
BH will look at the needs of an ageing population and transforming its same day and integrated care services.

Barnet has one of the largest and fastest ageing populations in London. Over 58,000 people are aged 65 or older, and this is expected to grow by around a quarter in the next 10 years.
This presents a particular set of challenges; people living longer means that they need more care and support later in life, and access to mental health support and urgent and emergency care is vital.
“Improving the care we provide to our older patients really is everybody’s business,” said David Levy, clinical lead for elderly medicine (pictured).
“We have 11 medical wards, eight of which are geriatric wards, and we have 23 geriatricians which is one of the biggest specialties in medicine in the trust,” he said.
For elderly patients, spending a long time in hospital can lead to an increased risk of falling, sleep deprivation, catching infections and sometimes mental and physical deconditioning.
To address this consultants and frailty clinical practice group (CPG) teams have been based at the emergency department and other points of entry to the hospital. They are quickly identifying patients who are suitable for other forms of care, whether that be virtual or ambulatory pathways, or community-based care.
“Ageing well is about bringing care to the person’s locality or home where possible, as it is a much better experience for them,” David added.
Dementia nurse specialists are also occupying and stimulating admitted patients on wards, while a physio-led ‘keep me mobile’ programme is getting patients out of bed to prevent deconditioning.

Clinical and non-clinical teams leading urgent and emergency care at BH are in the process of transforming the way in which adult and paediatric patient care is delivered.
The aim is to ensure intervention happens at the right time and place to allow specialists, where appropriate, to assess, diagnose and treat patients on the same day of arrival, instead of admitting them to hospital.
To do this we are focussing on the following:
- Opening of BH’s urgent and emergency care new front door. This space will provide a modern and spacious environment for staff and patients and will house triage, urgent treatment, and same day emergency care (SDEC) services. This is due to be completed this summer.
- Developing SDEC services, with the aim of delivering the same benefits as inpatient care.
- Expanding partnerships with external stakeholders to create a fully integrated urgent care offer for patients, in particular virtual ward services. We are working with other local trusts to design and expand this so we can deliver safe care beyond our hospital wards.
- Improving outcomes for frail patients by reducing time spent in the emergency department (see story above). The plan is to wrap a multidisciplinary team around patients at the start of their ED journey, as well as discharge planning from arrival and to offer a more holistic approach by linking into community services.
Royal Free Hospital (RFH)
The RFH will focus on establishing the hospital as a national centre of academic and clinical excellence for rare diseases, and working with our partners to reduce chronic diseases and improve patient outcomes.
Improving the lives of people with rare disorders through innovative treatment and research is a key part of the RFH ambitions.
These disorders include amyloidosis, systemic autoinflammatory syndrome, haemophilia, immunology, lysosomal storage disorders, scleroderma and pulmonary hypertension.
When patients are referred from across the country to the rare disorders service, investigations are carried out on the same day, and many of the patients are keen to participate in clinical trials in order to push knowledge forward and help find improved treatment options.
Pratima Chowdary, clinical service lead for rare diseases, said the aim is to bring together support services that will enable them to deliver better patient care, increase research opportunities and create efficiencies.
“We want to bring together academic and clinical research to provide the best patient care using the latest diagnostics,” she said. “We also have logistical and operational support, like accommodation for patients who have to travel to come here, pharmacy and IT. It also means comprehensive care, supporting both the physical and psychological health of our patients.
“The set up will be similar for each service so if we can coordinate and pull together, that will benefit all of us.”
The rare disorders service is pulling together a strategy, setting out how this approach would work in practice – and part of this is providing a new IT system that will cater to the needs of the rare disorders services. It is hoped that the new system will be available in the coming two years.
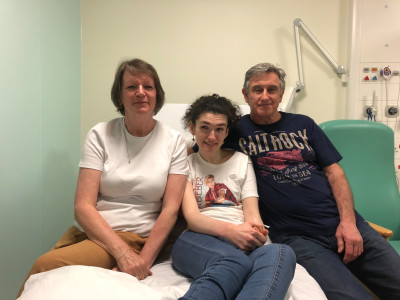
Ave Jones is one of the patients using the rare diseases service at the RFH.
The 22-year-old has been coming to the hospital for the past four years, having been diagnosed with Niemann-Pick disease type C (NP-C) aged 16.
People with the condition are unable to process large molecules within their cells, meaning fats accumulate around the brain, liver and spleen. It’s a progressive disease and symptoms include difficulties with mobility and dementia.
NP-C is caused by a rare gene mutation – neither Ava’s mother Debbie nor father Steve knew they were carriers for the gene until Ava’s diagnosis.
Debbie said: “Ava was initially diagnosed with hydrocephalus, which is a build up of fluid in the brain, and was treated for that. However, the symptoms continued after the treatment, and eventually she was diagnosed with NP-C.
“We wanted to be part of a clinical trial – it was why we decided to come to the Royal Free Hospital. It means coming here every six months for some tests, but we wanted to give Ava the best chance and to help expand the knowledge of this disease which has no cure.
“We are so proud to have Ava as our daughter,” Debbie said. “Despite everything that she has to deal with on a daily basis, she keeps smiling through and her smiles and laughter are infectious.”
Chase Farm Hospital (CFH)
CFH will continue to develop itself as a centre of excellence in elective surgery and improve early diagnosis and prevention through our group clinical services.

The lives of women across the country and north central London continue to improve one year on from the introduction of a new fibroid treatment at CFH.
The RFL was the first of four centres in London to begin offering Sonata, known as sonography-assisted transcervical fibroid ablation. The treatment alleviates symptoms of fibroids by using radiofrequency energy in the uterus.
It is minimally invasive and sees women across the UK travel to CFH, even from as far as 200 miles. Clinical studies have shown that it is effective, with 96% of women saying their symptoms improved within a year.
Consultant obstetrician and gynaecologist Mahantesh Karoshi carried out the first procedure in March last year.
Dr Karoshi said: “The Sonata treatment changes the lives of women who are troubled by fibroids. If patients meet the criteria, it is the least invasive treatment option for them to become symptom-free. Before, some women would need major surgery, whereas now, we can treat patients while talking to them and they can go home the same day.”
Stephanie Schandorf Gogo is the latest patient to undergo the procedure. She said: “I was having heavy and painful periods from my fibroids, but I didn’t want to put myself through surgery. I wasn’t sure if I would be able to have the treatment at first but luckily, Dr Karoshi told me he could treat some of my fibroids using Sonata. The procedure went really well.”
Giving everybody the same access to healthcare is central to improving the lives of the populations we serve. Early and equitable diagnosis within the RFL’s pathology services is one way we are doing
that for patients, no matter where they live.
This service involves a dedicated team of approximately 60 clinical and non-clinical staff who aim for quick turnaround times for tests and results. Around 80-90% of urgent samples and 70% of routine samples are processed within five working days – a critical metric in cancer pathways.
Within the service, each hospital within the group, including partner North Mid, maintains its own specimen reception area where samples are processed before being transferred to the main laboratory.
Here, the bulk of the processing occurs, and then glass slides are returned to the clinical team for reporting.
“A significant advancement in the field of cellular pathology this year is the adoption and implementation of ‘digital pathology’,” said Dr Dhili Arul, clinical director for pathology. “That is set to replace microscopes as the main way to examine samples, which should enhance efficiency and accuracy in diagnosis.”
In clinical biochemistry, the team includes consultants, junior doctors, and clinical fellows, who oversee laboratory operations and provide clinical interpretation services for clinicians and local GPs.
The RFL consultant team have also been part of developing an internationally recognised service for managing complex lipid disorders. They run extended clinics such as the HIV lipid clinic, joint paediatric lipid clinic, and joint fatty liver/lipid clinic.
“The team is also involved in conducting clinical trials related to the treatment of lipid disorders to advance medical knowledge,” Dr Arul added.
The combined efforts ensure all patients receive timely and accurate diagnostic assessments, which leads to earlier treatment and better outcomes.
 Translate
Translate