Sadly, patients with pancreatic cancer are often diagnosed at an advanced stage of their disease and as such, survival rates are much lower than for other forms of cancer.
In addition, treatment options have not changed significantly in many years and patients having access to clinical trials often represents their only hope.
At the Royal Free London, the pancreatic cancer service treats around 200 new patients each year.
Those with advanced disease are already being offered new combinations of treatment within clinical trials to see if they are more effective than the current standard of care.
But now, a number of new trials are opening at the Royal Free London which will recruit patients at all stages of disease.
These include the PRISM-1 study, which is looking to see if adding a new type of immunotherapy to chemotherapy works better than chemotherapy alone.
Opening soon are two new studies looking at whether combining new drugs with chemotherapy is beneficial. Ginisortamab is a new targeted cancer drug which blocks a specific protein in the body, thereby potentially allowing the body to stop the cancer spreading. The hope is it will also make the cancer cells more sensitive to chemotherapy.
The second trial, CRISTAL-APC, is assessing a tablet aimed at altering the balance of immune cells within tumours to try to make them more likely to be eliminated by the body’s own immune system.
For patients who have no other treatment options available, studies are also opening for therapies not previously tested in humans - or in only very few people. These include the HERTHENA study which is looking at a drug that enables chemotherapy to be targeted towards tumour cells specifically. The hope is that this may direct treatment to tumour cells while leaving non-cancer cells unaffected, reducing the risk of significant side effects.
The EMITT-1 trial is investigating a new drug aimed at making cancer cells more visible to the immune system. This is important for patients with pancreatic cancer, as the majority of these patients do not respond well to immunotherapy, despite significant progress with this treatment in other cancers.
Finally, pancreatic cancer patients who are suitable for clinical trials are now able to have a simple blood test to detect and analyse the DNA of their cancer. This is called a ‘liquid biopsy’ and is able to identify over 300 different cancer genetic abnormalities which may enable these cancers to grow. This has the potential to identify new targets for treatment or to improve selection for specific trials based on a personalised map of their cancer genome.
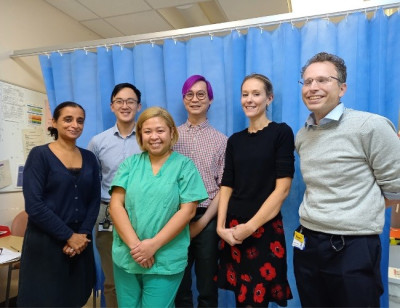
Dr Alexa Childs, consultant in medical oncology at the Royal Free Hospital and principal clinical research fellow at the Division of Immunity and Transplantation (UCL), pictured second from right, said: “Our aim is to ensure that patients with all stages of pancreatic cancer have the option to participate in clinical trials if they wish, and that we try to deliver these studies as close to home as possible.”
Dr Robert Goldstein, consultant in medical oncology at the Royal Free Hospital, pictured far right, added: “We hope to attract patients from across the region to take part in these exciting clinical trials which could ultimately pave the way to better outcomes.”
The trust’s pancreatic cancer service serves a population of 3.5 million from across NCL, Bedfordshire and parts of Essex and Hertfordshire.
November is pancreatic awareness month.
Pictured: Hepatobiliary oncology team
 Translate
Translate