This leaflet answers common questions about calf muscle tears. If you would like further information, or have any worries, please do not hesitate to ask your nearest clinician.

What is a calf muscle tear?
This is a soft tissue injury (sprain) to your calf muscle.
Healing
This normally takes approximately six weeks to heal depending on severity of the sprain.
Smoking will slow down your healing. We would advise that you stop smoking while your fracture heals. Talk to your GP for more information.
Pain and swelling
Your calf will be swollen and painful. Swelling is often worse at the end of the day. It is normal to have mild pain and swelling for three to six months after your injury. Taking pain medication, elevating your ankle, and using ice or cold packs will help. More information is on the next page.
Wearing your boot
You may have been given a boot, possibly with wedges under your heel to make you more comfortable. Wear the boot when you are standing and walking for the first two weeks. You can take it off at night and at rest. You are allowed to put weight through your leg. You may find it easier to use crutches in the early stages.
Exercise and activity
It is important to start exercises as soon as possible. Instructions are further down this page.
Follow up
We do not routinely follow up patients with this injury as they recover well with self-management. Please contact our team if after 12 weeks you still have significant pain or swelling, or if you struggle to wean out of the boot.

Caring for your injury: Weeks 1 to 2
Use with boot and/or wedges for comfort when walking. Try to stop using them as soon as possible. Start by gradually removing the wedges from your boot to lower your heel down.
You can remove the boot when resting and at night. Wear a long sock in your boot.
Using a cold pack will help with your pain and swelling. You can use an ice pack or bag of frozen peas wrapped in a damp towel. Put this on your ankle for 15 minutes every few hours. Make sure the ice isn’t in direct contact with your skin.
Try to rest your leg, especially in the first 24-72 hours. Raise your ankle on a stool or cushions so that it is above the level of your hip. This will help to reduce your swelling.
Exercises
Early movement of the ankle and foot is important to promote circulation and reduce the risk of developing a Deep Vein Thrombosis (blood clot). Do these exercises three to four times a day. Start straight away, you do not need to push into pain.

- Point your foot up and down. Repeat this 10 times.
- With your heels together, move your toes apart to turn the foot outwards. Repeat this 10 times. Do this movement gently within comfort.
- Make gentle circles with your foot in one direction and then the other direction. Repeat this 10 times.
Caring for your injury: Weeks 2 to 6
Try to stop using your boot and crutches. Start by walking without them around your own home. Build up to not using them outside and for longer walks. Wearing supportive shoes such as trainers will help.
Activity and exercise
You can gradually increase your level of activity. It is normal to still have some mild symptoms. Contact our team if you struggle to return to sport or exercise after 12 weeks.
Balance exercises: Start these two weeks after your injury
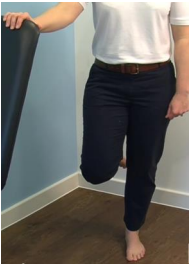
These exercises are for people who could stand on one leg before their injury.
-
Hold onto a firm surface in a safe space. Try to stand on one leg. Hold this for 30 seconds. Stop if you experience pain. When you can do this comfortably, try the next exercise.
-
Try to stand on one leg without holding on to a support. Try to hold this for 30 seconds. When you can do this comfortably, try the next exercise.
-
You can try these exercises with your eyes closed. Make sure you are always in a safe environment with a support to hold if needed.
Stretches: Start these three weeks after your injury

- Sit with your leg straight out in front of you. Put a towel or bandage around your foot and pull it towards you. Feel a stretch in the back of the calf.
- Point your toes down as far as they go, place the other foot on top and apply some pressure. This will stretch the top of your foot. Hold for 30 seconds.
I am struggling with my boot. What do I do?
The boot has a thicker sole; this can make you feel uneven. Make sure you wear a supportive shoe or trainer on your uninjured foot. This will reduce stress on other joints. If you need more advice, contact the Virtual Fracture Clinic.
Watch this NHS video on fitting your boot
I am diabetic, does this change things?
If you are diabetic please contact us to discuss your boot. This is particularly important if you have problems with your skin or sensation. We may provide you with a specialist diabetic boot.
Driving
You can return to driving when:
- You are no longer using your boot,
- You can walk comfortably and
- You can perform an emergency stop pain free.
Always test your ability to drive in a safe environment first.
Fitness for work statement
You can get a fitness for work statement from your GP or the doctor at your fracture clinic appointment.
What do I do with my boot and crutches when I no longer need them?
We are not able to use boots again. These should not be returned to the hospital. Crutches can be returned to the fracture clinic or emergency department (A&E).
 Translate
Translate