This leaflet answers common questions about digital ulcers in scleroderma. If you would like further information, or have any worries, please do not hesitate to ask your nurse or doctor.

What are digital ulcers?
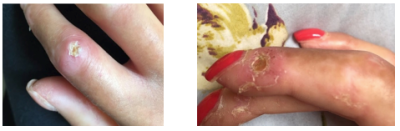
Digital ulcers (DU) are ulcers or wounds that develop on the fingers or toes of people diagnosed with scleroderma or systemic sclerosis (SSc).
Causes of digital ulcers
DU can be caused by Raynaud’s phenomenon. This is a condition where blood flow to the fingers and toes is temporarily reduced triggered by:
- Change of temperature eg. cold or stress)
- Sclerodactyly (tight skin)
- Contractures
- Trauma (e.g. knocking fingers on objects)
- Calcinosis (calcium deposits that develop under the skin in some people with SSc)
- Cracked or cuts
- Extremely dry hands.
Prevention
Unfortunately, most times DU cannot be stopped from developing. It is one of scleroderma complications. However, there are things that you can do to minimise DU.
- Keep your hands and nails clean.
- Keep your hands and feet moisturised and supple.
- Keep warm, use or put on warmth maintaining clothes or gadgets.
- Stop smoking.
- Use paraffin hand wax. If you have an open wound avoid using it directly instead use it over disposable gloves, it helps to keep blood vessels open, softens the skin and keeps it supple.
Make sure that your Raynaud’s medications (e.g. vasodilators which are medications that relax and widen blood vessels, while improving blood flow, e.g. losartan, nifedipine, sildenafil and others) are maximised. Wear comfortable well-fitting shoes with plenty of room in the toes, with natural lining and breathable.
How to recognise when a digital ulcer is developing
People experience the development of DU in different ways. Some report that several weeks before the DU appears they have pre-warning signs such as tingling on the area it is likely to appear and tenderness, others do not experience the signs. Some signs of a DU developing include warmth to the area, change of colour (mostly red), pain, tingling or itching?
What to do when you suspect a digital ulcer is developing
Make sure that you are taking your Raynaud’s phenomenon medication. Take pictures of the suspected area and continue if you notice noteworthy changes. Protect the area that you feel the ulcer will develop with a dry padded dressing to avoid knocking it by mistake. Contact our helpline on 020 7472 6200 if you are sure the ulcer will soon open or becomes unduly painful without opening.
What to do when it opens
Act quickly because complications such as infections and others can happen. Seek guidance from our helpline or your GP. Scleroderma is a rare condition and above 50 per cent of patients develop DU; be prepared to find your GP or practice nurse has never had to deal with one before. Keep it clean. You can clean it with clean gauze and some tap water or normal saline or prontosan wound irrigation solution or octenisan/octenillin.
Apply wound dressings that will keep the balance of dryness and moist (dressings mentioned below, while waiting for medical advice). If it becomes infected apply wound dressings that will help to get rid of the infection and you may need to be prescribed oral antibiotics. If it is taking longer to see your GP or its out of working hours and the DU is infected or the pain is increased, you might have to seek help from an emergency GP or local emergency services or 111.
If the DU is open and infected, a swab should be taken. If you suspect infection, act quickly. Signs of infection include increased pain and or throbbing, red, swollen, or puffy, warm to touch, accumulation of pus under the skin or pus oozing.
Avoid using Fucidin acid on digital ulcers; it may worsen the infection. Speak to your GP for suitable alternatives. Also, if the DU starts changing colour eg getting dark or surrounding skin getting continuously purple or blue, please contact us immediately.
Mostly wound dressings applied must be prescribed by the GP, pharmacist, or the hospital. But if you cannot access your GP or hospital immediately, some dressings such as hydrogel, hydrocolloid, mepore dressings can be purchased over the counter. Always seek medical advice as soon as possible.
Some dressings require a top cover dressing to hold them in place. Examples of dressings, not exhaustive of all wound dressings:
For non-infected ulcers
- Duoderm extra thin (no top dressing required)
- Activheal hydrogel
- Actiform cool
- Aquacel extra
- Jelonet
- Cutimed sobact hydrogel
- Kerralite cool
- Medicated manuka honey
- Flaminal gel
- Urgo Tul
- Sorbsan
Infected ulcers
- Aquacel Ag
- Inadine
- Medical grade honey
- Cutimed sobact gel
- Prontosan wound gel
- Silvercel
- Suprasorb A+Ag
- UrgoClean Ag
Caution should be taken when using wound dressings for an infected ulcer, seek advice on how to use them and for the duration. If unsure of how to use any of the dressings, please seek medical advice.
Dealing with pain from digital ulcers
Pain is a big issue in DU. It is important that you receive medically prescribed strong pain relief medications such as Buprenorphine patches. They are slow releasing pain killers, oxycodone/naloxone, morphine, fentanyl, and others. These medications should be taken with caution because they can result in constipation, other side effects and risk of addiction if taken over a long period of time. Speak to your GP about managing these side effects, such as using laxatives or adjusting your medication.
Sometimes EMLA cream which is a numbing cream may help to numb the area. Care should be taken on how to apply it onto the wound. This can introduce infection. Use clean gauze to apply the cream, but do not apply the cream directly from tube to the ulcer. Some dressings in the category for non-infected ulcer dressings above may reduce pain. It is a combination of different treatments that helps to reduce pain in DU.
Treatments for digital ulcers
Vasodilators
- Losartan
- Nifedipine
- GTN patches (prescribed with caution)
- sildenafil
- diltiazem
- and others.
Intravenous infusions
- Iloprost
- Prostacyclin (Flolan)
Pain killers
These are not exhaustive of all painkillers, and they are prescribed with caution but may include:
- Codeine
- Co-codamol
- Buprenorphine patches as they are slow releasing pain killers
- Tramadol
- oxycodone/naloxone
- morphine
- fentanyl patches
- and others
Debridement
A procedure to remove dead or infected tissue from a wound.
Wound dressings
As stated above, in dressing that can be applied.
Natural therapies
Please ask for our natural therapies leaflet for more information.
Botox
This is an injection that can improve blood flow to affected areas by relaxing muscles),
Hand and foot paraffin waxing
Therapeutic treatment to keep skin soft and improve circulation).
Amputation
A last resort is surgical amputation, although we do not advocate for this. It can cause other complications such as delayed healing or infection.
 Translate
Translate