This sheet answers common questions about having a laparoscopic cholecystectomy or surgery to remove your gallbladder. Your surgeon may have recommended you undergo an operation to remove your gallbladder, however it is your decision to go ahead with the operation or not. If you would like further information, or have any particular worries, please do not hesitate to ask your nurse or doctor.
In all cases, a doctor will explain the procedure to you and answer any questions you may have.

What is a gallbladder?
Your gallbladder is a small sac that is attached to the bottom of your liver. It stores and concentrates bile, which is a liquid produced by your liver. Bile has a number of functions, one of which is to help you absorb and digest fats. Bile enters your small intestine through your bile duct.
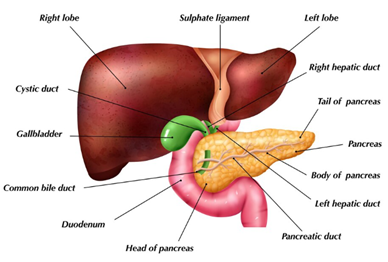
Fig. 1: Picture of the gallbladder, bile ducts and liver.
What is a laparoscopic cholecystectomy?
This is an operation to remove your gallbladder using keyhole surgery. A laparoscopic cholecystectomy may be performed to:
- remove troublesome gallstones
- remove any polyps or other abnormalities in the gallbladder.
Your gallbladder is not an essential organ. If it’s removed, bile will continue to flow into your intestines directly from your liver. Most people who have had it removed don’t notice a difference, however, some patients do experience looser stools after a cholecystectomy.
How is the procedure done?
You will be given a general anaesthetic where you will be asleep for the entire procedure. The surgery itself normally takes about 60 to 90 minutes but can last up to a few hours.
A special camera called a laparoscope is inserted into your tummy through a small incision made near your belly button. Gas is blown into your abdomen to allow us to get a clear view of your gallbladder. Your surgeon may make another two to three incisions for the keyhole surgical instruments to be used.
During the operation, the gallbladder is detached from the liver, its blood supply and the bile duct. It is then removed through one of the incisions already made in your tummy for the surgical instruments.
If it becomes unsafe or is not possible to continue your operation with keyhole instruments, an ‘open’ operation must be performed. This involves a larger cut under the ribs or up and down the centre of your tummy. The size of this cut is kept as small as possible but is typically 15-20cm in length, though can be considerably longer.
Your surgeon may decide to inject a dye (contrast) into your bile duct and take an x-ray or ultrasound scan during the surgery. If they suspect a stone is blocking your bile duct, they may try and remove it during the surgery or bring you back at a later date to have it removed in another way.
Occasionally, a plastic tube (a drain) is left inside your tummy at the end of the operation to allow any fluid that builds up in your tummy after the operation to escape and be collected in a bag. This is normally only needed for a few days and is removed on the ward before discharge, but your surgeons will explain this.
During the operation, we occasionally need to take photos or videos for your medical records to help with your diagnosis and treatment. We may also ask for your permission to use anonymised versions of these images for training other healthcare professionals and students. Images would not be used for any research unless you give express written permission for us to do so. You do not have to give your permission for us to use your images and your decision will not affect your care in any way.
As we are a teaching hospital, there may be student nurses, student doctors and other allied health care professionals involved in your care. Please let us know if you are not happy with this.
Where will my operation take place?
Gallbladder surgery is performed at:
- Chase Farm Hospital
- Barnet Hospital
- Royal Free Hospital
- Whittington Hospital.
The hospital where you have surgery may be different to where you had your outpatient appointment, or where you were admitted, to ensure your surgery is performed as quickly as possible.
Before your procedure
Tests prior to surgery
Your surgeon may decide you need further scans before putting you on the waiting list for surgery.
You will need to have blood tests to look at your liver function. If your liver markers are raised, this could mean a gallstone has moved into your bile duct. You may need to have these stones removed via an endoscopy before you have your gallbladder operation.
You will also need to attend a pre-operative assessment, where a nurse will check you are fit enough to undergo the surgery. This may involve a telephone appointment and tests such as an electrocardiogram (tracing of the heart rhythm), blood tests and occasionally an x-ray. Some people may need to see an anaesthetist or have more complex tests.
This process does occasionally identify previously undiagnosed medical problems and this can sometimes delay your operation.
Getting your consent
There are risks associated with any operation and your surgeon will help you balance the risks and benefits in your specific case to help you decide if you wish to proceed. If you are uncertain at any point, or do not understand something, please ask.
If you decide to go ahead, we will ask you to sign a consent form on the day of your operation. You are welcome to change your mind at any point during the process up to the point you are under anaesthesia. We are always happy to make another appointment to discuss things further should you wish it.
After your surgery
What to expect
Most patients will go home on the same day as their surgery. If there are any complications during the surgery or you have had an ‘open’ operation, you may have a longer stay.
Your wounds from surgery will normally be closed using stitches, skin glue, metal clips or a combination of these. Some stitches and all metal clips need to be removed around 10 to 14 days after your operation. Dissolving stitches or glue do not need removing.
Your wounds will then be covered by a dressing or left open (if skin glue has been used). If needed, you will be given a small supply of dressings and the nurse will show you how to dress your wound. Please notify us in advance if you have any allergies to any plasters or dressings.
Most people will experience mild to moderate abdominal pain after surgery, which is easily controlled with painkiller medication. Often, your surgeon will also use a local anaesthetic in and around your wounds to try and numb the area for when you wake up. This will wear off after several hours and by then you should be able to have other painkillers if needed.
You may notice some shoulder pain which is due to the gas inserted into your abdomen during surgery. After about two to three days, most of the discomfort should disappear. If this is not the case or the pain worsens, then urgently seek medical attention.
You can eat and drink as normal after your operation. It may take a few days before your appetite returns to normal. When you feel hungry, start with light frequent meals and then increase at your own pace. Some people find that they do not tolerate fatty foods as well as they used to.
When can I have a bath or shower?
If you have skin glue, you can shower and bath straight away. Please pat the skin dry and do not pick the glue off. The glue will fall off naturally once the skin has healed sufficiently.
If you have had stitches or metal clips used, please make sure you keep your wounds completely dry for the first 48 hours after your surgery. If possible, avoid having a bath or swimming within the first week, as this increases the likelihood of infection. Please avoid standing with the water spraying directly on your wounds within the first week.
After the first week, you can have a bath or shower as normal. Pat the wounds gently when drying. Avoid using creams or ointments on your wounds until they have fully healed.
Getting home
Wherever possible, patients are required to make their own way to and from hospital appointments. If your medical condition affects your ability to travel independently (including with the help of friends, relatives or carers), please call the hospital transport department on 0333 240 4909 to see if you qualify for hospital transport.
Returning to normal activities
You can return to your normal activities when you feel comfortable. You should avoid heavy lifting and vigorous exercise, such as running, for at least four weeks. You should gently build up your exercise as you feel able.
If you have had an ‘open’ operation, we suggest avoiding heavy lifting for two to three months.
When you can drive
Before driving, you should ensure you:
- are not taking medication that can make you drowsy or slow your reaction time
- can perform a full emergency stop without any pain
- have the strength and capability to control the car
- will be able to respond quickly.
You should check with your car insurance company as they may have specific restrictions in their small print. Please be aware that driving while unfit may invalidate your insurance and be a criminal offence.
Returning to work
You can return to work as soon as you feel up to it. This will depend on how you are feeling and the type of work that you do (e.g. if you are involved in manual labour or heavy lifting, you need to avoid straining for at least four weeks).
When should I seek medical advice after surgery?
In general, we would expect you to get better day on day after your operation. If this is not the case, or if you experience any of the following, then seek medical advice:
- excessive pain
- nausea and vomiting or your abdomen feels larger than usual and you are not able to hold anything down
- persistent or considerable bleeding from your wounds
- a high temperature (38°C / 100°F or above)
- you feel cold/shivery/unwell
- difficulty passing urine
- redness, tenderness and pain spreading from one of your wounds
- pus coming from your wound
- yellowness of the skin or eyes (jaundice).
In the first instance, you can contact your GP or the hospital ward if you need advice. If you are unwell and think it is an emergency, please call 999 or go straight to your nearest emergency department.
Follow-up or further treatment
For the majority of people, once their gall bladder is removed, no other treatment or followup is required.
Occasionally, you may be offered a telephone or clinic appointment to discuss the results from the examination of your gallbladder after surgery. This does not mean we have identified a specific problem and may be just so we can assess how you have recovered from the surgery.
What happens to my gallbladder after it’s removed?
Your gallbladder will be sent to a pathologist for examination. Your doctor will receive a full report from the pathologist after two to three weeks. If there are any further issues that need to be discussed with you, your doctor will contact you.
You may be asked if you are willing to allow researchers to look at your gallbladder to see if they can find ways to help patients in the future.
If you give your permission, any tissue not needed for your treatment or diagnosis could be used by researchers to help improve care or find new scientific discoveries. This can include genetic testing on the tissue and researchers may ask for access to your medical records. All research will only be carried out if it has received ethical approval from a research ethics committee.
You do not have to agree to participate in research and your decision will not in any way affect the care and treatment we offer you.
Risks and side-effects
While overall this is a safe operation, there are some important risks that we need to make you aware of. On average:
- There is a one in 1,500 risk of death, but the risk could be significantly increased depending on any other medical conditions you may have.
- There is a one in 300-400 risk of bile duct injury and one in 100 of bile leak following the operation. This may require further procedures or even major surgery to repair it.
- For patients with gallstones, there is a four in 100 risk of a stone escaping your gallbladder into your bile duct during the operation or stones being found in the bile duct.
Other risks include:
- If it is unsafe, surgeons may decide not to remove all/any of the gallbladder.
- Other structures in your tummy (such as bowel, the pancreas, liver, blood vessels) can be damaged during the operation and may require surgery to fix.
- There is always a risk that bile or stones from your gallbladder can be spilt inside your tummy and cause infections. We take every possible precaution to wash this out and/or remove them.
- There is a small risk of bleeding, infection and hernia formation following this procedure. We will ask you whether you are willing to accept blood as an emergency and please tell us in advance if you are not willing.
- Peripheral nerve injury can occur due to lack of movement for a long period of time after surgery.
- Complications such as wound problems, infections (e.g. chest/wound/intrabdominal/urinary), adhesions, hernia, deep vein thrombosis and pulmonary embolus can occur and will need treatment.
- Up to one in five patients may have persistent pain or discomfort. If your symptoms persist for two to three months after surgery, please contact your GP or surgical team.
- Some patients experience loose stools, bloating, heartburn, nausea/vomiting and pain after having their gallbladder removed - this is sometimes called post-cholecystectomy syndrome. These symptoms may be temporary or persist.
Risks of general anaesthetic
Although serious problems are uncommon, risks of general anaesthetics cannot be removed completely. The risk to you as an individual may be higher depending on previous problems with anaesthetics, other medical conditions, personal factors (such as smoking or being overweight) or if your surgery is complicated/performed as an emergency.
Very common and common side effects (1 in 10-100 people)
- feeling sick and vomiting after surgery
- sore throat
- dizziness
- blurred vision
- headache
- bladder problems (e.g. not being able to pass your urine)
- damage to lips or tongue (usually minor)
- itching
- aches, pains and backache
- pain during injection of drugs
- bruising and soreness
- confusion or memory loss.
Uncommon side effects (1 in 1000 people)
- chest infection
- muscle pains
- slow breathing (depressed respiration)
- damage to teeth
- existing medical condition getting worse
- awareness (becoming conscious during your operation)
Rare and very rare complications (1 in 10,000-100,000 people)
- damage to the eyes
- heart attack or stroke
- serious allergy to drugs
- nerve damage
- surgery equipment failure.
Deaths caused by anaesthesia in the UK are very rare (probably about five deaths for every million anaesthetics).
Alternatives to laparoscopic cholecystectomy
This depends on why you are being offered surgery to remove your gallbladder and you should discuss this in more detail with your surgeon.
Other short term gallstone treatment options can include:
- medication to dissolve small, non-calcified gallstones in a functioning gallbladder
- reducing gallstone symptoms by avoiding fatty goods and using painkillers
- antibiotics for gallbladder or bile duct infections
- camera test to remove stones lodged in bile ducts.
If the reason for surgery is to remove a polyp or an abnormal area within the gallbladder, there is no alternative treatment option. This is because the gallbladder needs to be looked at under a microscope to decide whether any further treatment is required.
What will happen if I decide not to have the operation?
If you decide not to have the operation:
- Your gallstones may not cause you any symptoms.
- If you have already had symptoms, it is likely that these will continue from time to time.
- There is a small risk of serious life-threatening complications such as pancreatitis, jaundice or severe infection (sepsis).
 Translate
Translate