This leaflet answers common questions about holmium laser enucleation of the prostate (HoLEP). If you would like further information, or have any worries, please do not hesitate to ask your nurse or doctor.
In all cases, a doctor will explain HoLEP to you and answer any questions you may have.
In most cases it will be possible for a friend or relative to accompany you for all or part of the procedure. Please ask your nurse or doctor.

What is the prostate and why is HoLEP recommended?
The prostate is a gland located just under the bladder which surrounds the urethra (water-pipe). When the prostate gets bigger it can compress the urethra, making the channel for urine to pass through smaller.
This can lead to symptoms that include:
- Straining to pass urine.
- Waking up several times at night to urinate.
- An urgency to urinate.
- Needing to pass urine frequently in the day.
In severe cases the prostate blocks off the urethra completely and the person cannot pass urine. This is called ‘urinary retention’. A catheter (a long straw-like tube) is inserted into the urethra and is used to drain the bladder.
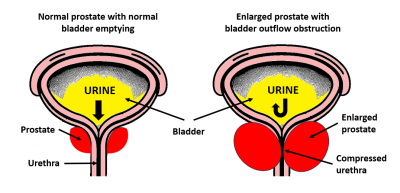
- The above left diagram shows a normal prostate (in red) with the bladder emptying normally.
- The above right diagram shows an enlarged prostate (in red) compressing the urethra and obstructing the flow of urine.
Before your procedure
At least 6 weeks before surgery, we recommend starting regular pelvic floor exercises. This is to reduce the leakage of urine (incontinence) after surgery. The more you exercise your pelvic floor, the less likely it is that you will suffer incontinence after surgery.
Access an online video explaining how to do pelvic floor exercises. Please note that this video was prepared for patients undergoing robotic prostatectomy (prostate removal for cancer). However, the exercises are also applicable to patients undergoing HoLEP.
The pre-operative assessment team will advise you on any medications which need to be stopped before the procedure and how many days before the operation you will need to stop these tablets.
For HoLEP at Chase Farm Hospital you will go home on the same day, so please ensure you have someone to drive you home and be at home with you that night. For HoLEP at Royal Free Hospital you will go home the next morning.
On the day of your procedure
You will be reviewed first by a nurse who will check your vitals and your urine for an infection. Your Urologist will go over the procedure with you and go through the consent form. You will either be put to sleep (a general anaesthetic) or have a needle in the back to numb you from the waist down (a spinal anaesthetic) and the Anaesthetist will discuss these with you.
During the procedure
During a HoLEP, a telescope is inserted into the urethra and a laser is used to remove most of the prostate, leaving behind the capsule. It is like removing the fruit from an orange and leaving behind the peel. This then provides a wide-open channel to allow your urine to flow more freely and improve your bladder emptying.
Below are the key steps of the procedure itself:
- A telescope is inserted through the penis and into the bladder.
- Laser fibre is passed through the telescope and used to peel the prostate away from its capsule.
- The removed prostate is then flushed into the bladder using the telescope.
- An instrument is then passed through the telescope to morcellate (chop up) the prostate tissue within the bladder.
- The pieces of prostate are then suctioned out of the bladder and sent to the laboratory for analysis.
- Any bleeding points within the cavity where the prostate used to be are lasered or diathermied to stop bleeding.
- A catheter is inserted.
- Irrigation is started, which is where water is flushed continuously into the bladder through the catheter. The water continuously comes out through another channel in the catheter into a bag.
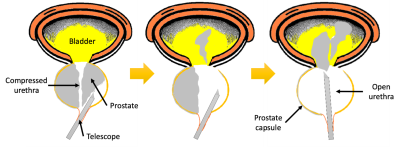
- The left image shows the telescope inserted into the urethra and the laser being used to shell out the prostate (in grey).
- The middle image shows the prostate being pushed into the bladder.
- The right image shows the rest of the prostate being into the bladder before it is chopped up and suctioned out.
The procedure usually takes around two hours but can take longer depending on the size of the prostate.
After your procedure
You will wake up on the recovery ward with a catheter in place with irrigation running. Later, you will be reviewed by a member of the team to explain how the operation went and review the catheter.
At Chase Farm Hospital, we will usually stop the irrigation and allow you to go home after a couple of hours. Rarely it will be too bloody to stop the irrigation. If that is the case, we will keep you in hospital for a night with the irrigation running until it clears.
Most patients operated on at Chase Farm Hospital will go home on the same day as the surgery with the catheter in place. We will make an appointment for you to come back to clinic two days later to have your catheter removed. For patients who have other complex illnesses, we will perform your surgery at Royal Free Hospital and aim to discharge home after at least a one-night stay in hospital.
Once your catheter is removed, your urine may be red for up to 4 weeks after your surgery. It is important to drink around 2 to 3 litres of water per day unless you have been previously advised otherwise by a doctor. If you are passing large blood clots or struggling to pass urine, then you should attend your nearest Accident and Emergency department.
After the catheter is removed, it is important to continue your pelvic floor exercises to prevent incontinence. Some incontinence is normal up to 3 months after surgery and you may need to use pads.
Risks and side-effects
All operations carry some risk of side-effects. Some risks are more likely or less likely, and this can vary from patient to patient. If you have any questions about the side-effects from your surgery, please speak to your surgeon about them and they would be happy to discuss.
|
Common side-effects |
Risk |
|---|---|
|
Mild burning and stinging when passing urine. |
Almost all patients |
|
Dry orgasms (no semen is produced during orgasm. Instead, semen goes back into the bladder and comes out when passing urine.) |
Almost all patients |
|
Blood in the urine up to 4 weeks after surgery |
Almost all patients |
|
Failure to pass urine after catheter removal requiring re-catheterisation and removal after 1 to 2 weeks. |
10-15% |
|
Short term incontinence. |
50% |
|
Occasional side-effects |
Risk |
|---|---|
|
An incidental finding of prostate cancer. |
5% |
|
Injury to the urethra (water pipe). |
5% |
|
Erectile dysfunction. |
Less than 5% |
|
Failure of the procedure to treat all your symptoms. |
1 in 50 to 1 in 250 patients |
|
Rare side-effects |
Risk |
|---|---|
|
Permanent incontinence. |
Less than 2% |
|
Needing to do the procedure again because of regrowth of the prostate. |
Less than 1% |
|
Making a hole in the bladder requiring a surgical repair. |
Less than 1% |
|
Needing to go back to theatre or have a blood transfusion because of bleeding. |
Less than 1% |
|
Needing a second stage procedure. |
Less than 1% |
|
Converting to an open operation (a cut down the tummy). |
Less than 1% |
Follow-up appointment
An appointment will be made with a member of the urology team approximately three months after your surgery. Before the appointment a nurse will see you to measure your flow rate. This will involve you passing urine into a container and measurements such as how quickly you pass urine and whether you completely empty your bladder will be taken. You will also need to be given a questionnaire called the IPSS (International Prostate Symptom Score) to complete. The results of this questionnaire, along with your flow rate, will be discussed at your appointment.
Alternatives to HoLEP
The alternatives to undergoing a HoLEP are below:
Transurethral resection of the prostate (TURP)
Here, the prostate is ‘shaved’ from the inside. There are many other new techniques available such as rezum, urolift, aquablation, or green light laser prostatectomy.
Prostate artery embolization
A local anaesthetic procedure to block off the blood supply to the prostate and shrink the size of the prostate.
Catheterisation
You may wish to be fitted with a catheter to drain the bladder continuously. This can either be a ‘urethral’ catheter, which is a tube inserted into the penis to drain the bladder, or a ‘supra-pubic’ catheter which is a tube inserted through the tummy to drain the bladder. A third option is to perform self-catheterisation where you insert a straw-like tube into the bladder to drain it and then remove the tube immediately afterwards.
Medications
Drugs for bladder outflow obstruction such as tamsulosin and Finasteride, or drugs for bladder overactivity such as solifenacin and mirabegron can all help with urinary symptoms.
Observation
No medications or surgery but simply managing symptoms through lifestyle changes such as stopping bladder irritants (caffeine, alcohol, fizzy drinks, spicy food).
Thank you for taking the time to read this information leaflet. If you have any further questions, please do not hesitate to discuss this with your surgical team.
 Translate
Translate