This leaflet answers common questions about preventing pressure ulcers. If you would like further information, or have any worries, please do not hesitate to ask your nurse or doctor.

What is a pressure ulcer?
A pressure ulcer is damage to the skin and/or underlying tissue, usually where bones are close to the surface of the skin (also known as a ‘bony prominence’). It is sometimes called a pressure sore or bedsore. One of the myths of pressure ulceration is that the skin must be broken. However, pressure ulceration can occur with the skin intact or broken.
For this reason, it is important to observe for the early signs of pressure damage which usually, but not always, include:
- Redness. People with darker skin tones may observe changes to the colour and texture of the affected area of skin
- Heat
- Pain
- Excess moisture to the skin, rash, and soreness if incontinent.
Pressure ulceration usually occurs over bony prominences such as the heels, hips, elbows, or bottom. This type of damage can be caused by sitting or lying for long periods of time in the one position. Direct pressure can cause damage and ischaemia (a restriction in blood supply to tissues, causing a shortage of oxygen that is needed to keep tissues alive).
This can affect the blood flow and lymphatics (an important part of our vascular and immune systems), damaging the skin and potentially damaging underlying muscle and bone.
Areas at risk of pressure ulceration
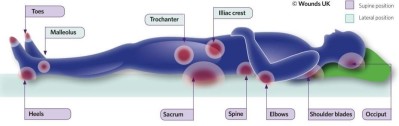
Other pressure points to monitor: chin, between the knees, bridge of nose, ear, and clavicle.
Who is at risk of developing a pressure ulcer?
Anyone can develop a pressure ulcer, but some people are more predisposed. You are at high risk if you:
- Already have a pressure ulcer or have had a pressure ulcer before.
- Have difficulty with your mobility or are unable to change your own position when in a bed or chair.
- Have reduced feelings in any part of your body, arms, or legs.
- Have incontinence.
- Have a poor appetite or have lost your appetite, or if you do not drink enough fluids.
- Are an older adult, are experiencing increasing frailty or have a long-term condition and suffer with ill health.
- Are a wheelchair user.
What can you do to protect against pressure ulcers?
Inspect your skin
Your skin should be checked at least once every day at home or more regularly in hospital. Ask your nurse, carer or family member to do this for you.
Look out for any pain, changes to the skin colour or if the skin feels hotter or colder and does not return to its normal colour or temperature when you have taken your weight off it. You may find that a hand-held mirror may help when looking at difficult to reach areas.
Do not continue to lie or sit on skin that appears to have changed. Choose a position that takes the weight off this area. If you can do so when sitting, regularly and safely move yourself in your chair.
Keep moving
Change your position regularly. If you can stand and walk, try to do this regularly. If you spend time sitting in a chair, try to lift your bottom to relieve the pressure hourly.
Where do pressure ulcers develop when seated?
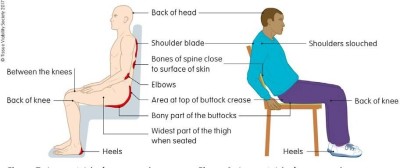
(Image ©Tissue Viability Society, 2018)
When you are in bed remember to change your position. If you are cared for in bed and are unable to change your own position, your nurse, carers or family will need to assist you with this.
Find out how often you need your position to be changed so that you can remind your nurse, carer of family.
Protect your skin
Avoid using soap and perfumed products and talcum powder on the skin as this will increase dryness and irritation.
Ensure after washing that your skin is absolutely dry. Remember to pat and not rub the skin. You may wish to speak to your nurse or doctor about a suitable soap substitute or emollient to wash. Moisturise your skin to keep it healthy and supple.
If you have incontinence, there are skin friendly pH balanced cleansers that your nurse or doctor may recommend you use. Keeping the skin clean and healthy is an important part of preventing pressure ulcers.
Eat well
Eating a well-balanced diet and keeping well hydrated is important to maintain good skin health and prevent pressure ulcers. If you have noticed a reduction in your appetite or change in weight, speak to your doctor or nurse as soon as possible.
For more information see NHSI (2018a) Improvement Guide: Eat well, drink well and keep the skin well and the five top tips to prevent pressure ulcers NHSI (2018b).
What can you do if you develop a pressure ulcer?
Seek advice from a healthcare professional such as your nurse or doctor. They will arrange an assessment of your skin and the pressure ulcer.
They will also put in place a pressure ulcer management plan to help to heal the wound which will include on-going skin assessments, wound dressings and may include specialist equipment such as a pressure reducing mattress and/or a pressure reducing chair cushion.
If your mobility is poor or you are unable to change your position in a chair or bed, you may need help, and this will be discussed with you.
Contact a healthcare professional as soon as you are aware of the pressure ulcer as early treatment may prevent the ulcer from getting larger or deeper. Deeper pressure ulcer can take a long time to heel and may require an admission to hospital.
- Barnet Hospital
Telephone 020 7794 0500, extension 64139 - Royal Free Hospital
Telephone 020 7794 0500, extension 38882
 Translate
Translate