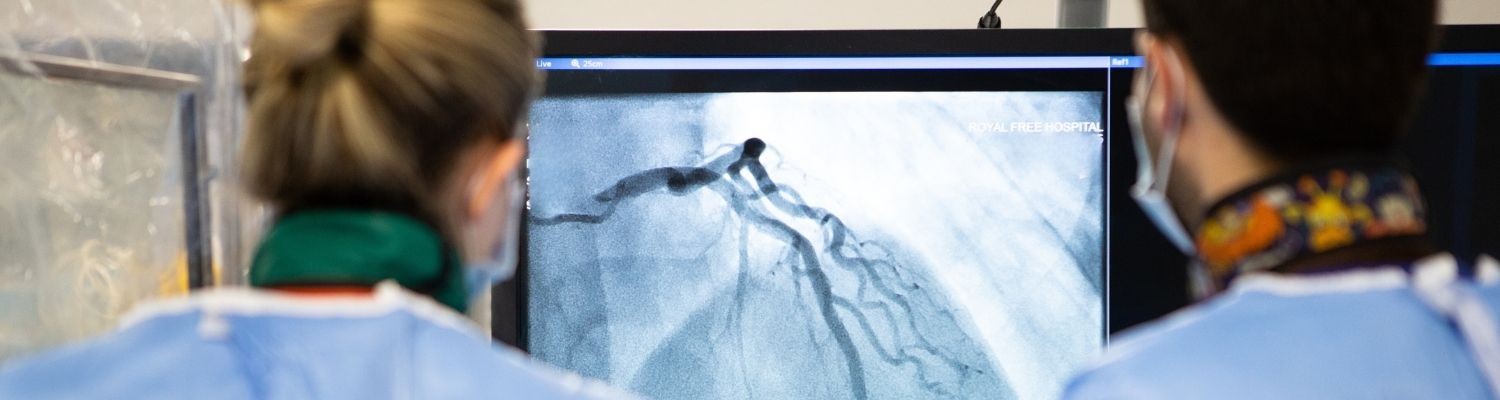
A cardiac CT scan offers a non-invasive method of evaluating the heart arteries and other structures within the heart using X-rays.
We offer this service in our radiology department, with reporting of the scans performed jointly by expert cardiologists and radiologists. They are supported by a team of highly trained radiographers.
The Royal Free Hospital performs over 1,000 scans per year using state-of-the-art technology, and has some of the lowest rates of patient radiation exposure in the country.
If you need to rearrange your appointment, please call the radiology department on 020 7830 2036 or email rf-tr.
If you need to contact the cardiology department regarding your scan, please call 020 3758 2069 or email rf.
Cardiac CT is a specialist scan and would be requested through the hospital by one of our cardiology team.
A cardiac CT (computed tomography) scan uses multiple X-rays form different angles to construct detailed three-dimensional images of your heart and the surrounding structures.
New scanner and computer technology allows detailed assessment of the coronary arteries, with the aid of an injection of a colourless dye (contrast) through a small cannula.
Your doctor or specialist nurse may request a cardiac CT for the following reasons:
- To check your coronary arteries for calcium and plaque build-up that cause narrowing or blockages. This is the most common reason for the scan and is often used for the investigation of chest pain.
- To assess your heart valves.
- To check the main blood vessels coming off the heart, such as the aorta, to look for aneurysms or tears within the artery (dissection).
- To plan for procedures such as trans-catheter/percutaneous (keyhole) procedures such as angiography or valve replacement.
- To look for any complications following a cardiac procedure.
- To look at the sac surrounding the heart for fluid, thickening or calcification.
- To see and assess any masses or tumours within or near the heart.
You will receive an appointment to attend the CT scan in the radiology department at the Royal Free Hospital. You should come to the radiology reception desk and check in. After this, you will be called in for your test.
While we ask you not to eat a heavy meal prior to the test and to refrain from caffeine for around 12 hours before attending, there is no need to starve for the test and we ask you remain hydrated before coming.
You may be prescribed medication (such as beta-blockers) prior to attending by your specialist or GP, in order to lower your heart rate in preparation for the test.
If you are prescribed this medicine, it is important you take it on the days leading up to the test and the morning of the scan. This ensures the heart rate is regulated and that we can obtain the highest quality pictures of your heart. Do not use drugs such as sildenafil (viagra) or similar medication on the day before or the day of the examination.
We would recommend you leave jewellery at home and wear comfortable clothes, as you will be asked to change into a hospital gown.
The vast majority of scans are performed with a dye (contrast) so one of our team will insert a cannula into your arm before the test. This will be used to administer the dye, but also additional medication to lower the heart rate immediately before the procedure. The dye allows the blood vessels and the heart to be seen clearly for the procedure.
Our team will explain the scan to you and also ask you some questions about your past cardiac history. These will include questions about any previous heart procedures (eg stent procedures), surgery (eg bypass or heart valve surgery), any history of heart valve disease or heart failure, previous asthma, and if you have any allergies to the dye (contrast).
We also ask if you consent for your images to be sent for specialist analysis to a team (Heartflow) outside the hospital. This is so they can perform a highly specialised analysis of the heart arteries, to assess the impact of any narrowing of your arteries.
You will be asked to lie on your back on a table that moves in and out of scanner. Our radiographers will clean three small areas on your chest and stick electrode patches. These electrodes will be attached to an ECG monitor which will record the heart’s electrical activity during the test and allow the scan to be performed at the right time.
At this time, the team will assess your heart rate and take your blood pressure. Depending on these, a doctor may give you additional medication (intravenous beta blocker) through your cannula, to lower your heart rate further.
The doctor may also give you some medication as a spray under the tongue (nitrate spray). This is in order to dilate or increase the size of the arteries around the heart to allow them to fill more with the dye and allow better imaging of the heart arteries. The spray may give you a slight headache and occasionally can make you feel a bit light-headed. These symptoms will only last a short period of time.
Occasionally, we are unable to lower the heart rate sufficiently to perform a diagnostic scan. In this instance, you will either be given a prescription for some medication to take before attending and the scan re-booked, or the doctor will notify the team that requested your scan to request a different test to assess your heart.
You will lie on the scanner table with your arms raised over your head for the duration of the scan. You will not be completely enclosed in the scanner as your head and feet will stick out of either end.
The radiographers will then ask you to practice some breathing manoeuvres that will take place before during the test. The machine will ask you to take a breath in and hold it for a few seconds, before asking you to breathe normally.
You will be connected to the machine that administers the dye through your cannula.
The radiographers will speak to you from the control room behind a glass window so they will see and hear you all the time. They will speak to you through a microphone and explain what is happening.
The table you are lying on will move into the scanner and the machine will ask you to take a breath and hold it a couple of times during the planning of the scan.
Once this is complete, the dye will be injected through your cannula and you will feel a warm sensation through your body as the contrast circulates. It will feel like you will want to pass urine but this sensation will pass very quickly.
You will be asked to hold your breath and the scanner will take the images of your heart. It is important you stay as still as possible during the scan as movement can cause the image to become blurry. The scan itself takes a matter of seconds.
The doctor will review the scans to ensure they are of good quality to be analysed and then the radiographers will return to the room and check how you are. Very occasionally, the scan needs to be repeated if it is not clear enough.
You will be asked to come off the table, disconnected from the machines and heart monitor, and you will be able to change back into your own clothes.
If you have had medication given to you during the test through your cannula, you will be kept in the waiting room for 10 to 20 minutes and your blood pressure and heart rate will be rechecked. If you have not received any additional medication, you will be free to go.
You will be able to go back to normal activities and eat normally. We encourage you to drink plenty of water after the scan for the rest of the day to help flush the dye through your kidneys.
The scan will then be reported by both a cardiologist and a radiologist. The report will then be made available to the doctor or nurse who requested the test, who will then inform your GP and you of the result by letter and decide on the next steps in your care.
Cardiac CT is a very safe and low-risk procedure. There are, however, some people who have problems with the dye and other medication we use during the procedure.
We do not perform the scan if you are:
- pregnant
- have an allergy to the contrast agent (dye)
- have a history of advanced kidney problems and this has not been discussed with your cardiologist or kidney consultant
If you are aged over 60, we require you to have had a kidney blood test prior to the procedure.
The vast majority of people have no problems with the contrast agents that we use. Occasionally, a small number experience an adverse reaction mainly due to the iodine within the contrast. Please let us know if you have had a reaction to the dye before or have an allergy to iodine or to seafood.
Some people developing itching, nausea and vomiting, sneezing or a rash after the injection. These symptoms generally go away without any specific treatment, but sometime antihistamines or steroids are used.
There are rare occasions where a more serious allergic reaction to the contrast may occur. This can lead to breathing difficulties and may require medication and treatment to reverse the symptoms of a potentially life-threatening reaction.
If you have diabetes or kidney disease, you may need additional fluids before and after the test to help remove the iodine out of your body. If you have advanced kidney disease, CT is only performed following a review by a member of your specialist team.
The CT scan is an X-ray test, so requires the use of radiation. This carries a tiny risk of cancer over time.
The cardiac scans we performed have some of the lowest radiation doses in the country, due to the type of scanner we use. The doses are comparable to other types of CT scans that are offered routinely. They are also similar to the level of background radiation you would naturally be exposed to in one year of living in the UK.
You may receive medication to slow down your heart rate for the test. This is done to ensure we obtain the clearest possible images of your heart. Medication may be prescribed before you come for your scan, or given to you through the cannula when you attend.
If you have a diagnosis of heart failure, asthma or chronic obstructive airways disease (COPD)/emphysema, please let your specialist know.
If you normally use an inhale, we would suggest you bring this with you when you attend for your test.
The scans are reported by a cardiologist and a radiologist who make a thorough assessment of your heart. The radiologist will also report on the surrounding structures such as the lungs and bones.
The report will be made available to the doctor or specialist nurse that has requested the test, who will then report that back to you and your GP.
They will then decide if any follow-up is required in the specialist clinic, or if you can be discharged to your GP with appropriate advice.
 Translate
Translate